Abstract
Introduction: Allogeneic hematopoietic cell transplant (alloHCT) represents a potentially life-saving treatment for patients with both malignant and non-malignant diseases. AlloHCT related costs accounted for the most rapid increase in total hospital cost, with a growth rate of 84.9%, from 2004 to 2007 according to an Agency for Health Care Research and Quality report (Stranges, HCUP Statistical Briefs, 2006). Higher cost has been associated with use of alternative donor sources and post-transplant complications. Transplant care improvements have led to better outcomes (Gooley, NEJM, 2010) but the effect on cost is not known.
Methods: We obtained data for 240 patients who received an alloHCT at Columbia University Medical Center between 1/1/05 and 6/30/16 and were <21 years old at the time of alloHCT for the first year post-transplant. Patient clinical characteristics and outcomes were obtained from retrospective review of medical records. Hospitalization cost data was estimated from charges obtained from the Pediatric Health Information System (PHIS) database using hospital specific cost-to-charge ratios and adjusted for inflation. To analyze changes over time, patients were divided into three time periods 2005-08 (n=103 patients), 2009-12 (n=73 patients), 2013-16 (n=64 patients). Primary outcomes were overall survival (OS), transplant related complications (liver injury: total bilirubin >2, kidney injury (decrease in creatinine clearance by >50%), viremia, bacteremia, acute graft-versus-host-disease (aGVHD) and inpatient resource utilization. The comparisons among groups were carried out by Kruskal-Wallis test for continuous variables and Chi-square test for categorical variables.
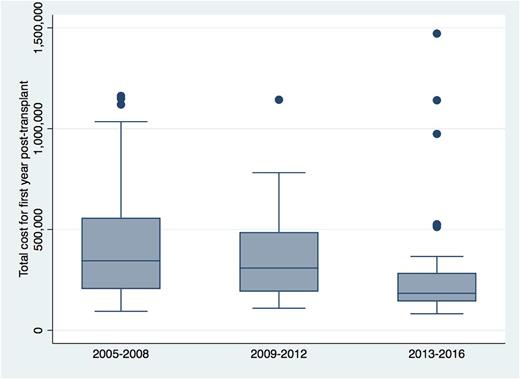
Results: There were no differences over time with respect to patient age, sex, related vs. unrelated donor, myeloablative vs. reduced intensity conditioning. The median age was 10.32 (range 0.34-20.96) years. There were significant differences in number of patients with nonmalignant disease (2005-08: 42%, 2009-12: 45%, 2013-16: 63%, p=0.027) and full HLA match (2005-08:44%, 2009-12: 56%, 2013-16: 64%, p=0.026). Liver injury in the first 30 days occurred in 2005-08: 30%, 2009-12: 32%, 2013-16: 27%, p=0.81. Kidney injury occurred in the first 30 days in 2005-08: 28%, 2009-12: 40%; 2013-16: 27%, p=0.22 and in the first year post-transplant in 2005-08: 85%, 2009-12: 78%, 2013-16: 66%, p=0.011 respectively. Viral infections were 2005-08: 27%, 2009-12: 51%, 2013-16: 41%, p=0.006, and there was a significant difference in mean days with bacteremia 2005-08: 3.4, 2009-12: 2.1, 2013-16: 1.8, p<0.001. There was also a significant difference in incidence of aGVHD 2005-08: 33%, 2009-12: 45%; 2013-16: 20%, p=0.009. There was no difference in OS 2005-08: 69%, 2009-12: 74%, 2013-16: 81%, p=0.21. There were significant differences in hospitalization lengths and costs between the three time periods with the lowest median inpatient days and costs for the 2013-16 group. The median lengths of transplant admission were 2005-08: 52 days, 2009-12: 48 days and 2013-16: 41 days (p<0.001). The median total inpatient days for the first year post-transplant were 2005-08: 98 days, 2009-12: 93 days, and 2013-16: 53 days (p<0.001). The median cost of the first transplant hospitalization was 2005-08: $184,450, 2009-12: $156,020, 2013-16: $130,244 (p<0.001), and median total one-year inpatient cost was 2005-08: $344,424, 2009-12: $308,826, 2013-16: $181,205 (p<0.001). The median cost per day survived was 2005-08: $433, 2009-12: $371, 2013-16: $202 (p<0.001). Stratifying the cohort by disease type and donor source, the median cost of alloHCT for matched related donors was 2005-08: $271,674, 2009-12: $213,546, 2013-16: $163,251 (p=0.012), for unrelated donors was 2005-08: $377,484, 2009-12: $380,211, 2013-16: $219,208 (p=0.007), for malignant diseases was 2005-08: $341,989, 2009-12: $363,676, 2013-16: $219,208 (p=0.07) and for non-malignant diseases was 2005-08: $344,424, 2009-12: $262,814, 2013-16: $184,280 (p<0.001).
Conclusion: Cost of alloHCT for pediatric patients treated at our center from 2005 to 2016 appears to have decreased. This is most likely related to improved care practices stemming from various quality improvement projects, leading to decreased lengths of hospitalization as well as decreased incidence of complications most significantly kidney injury, aGVHD and bacterial infection.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal